The family left behind
ANativeAmericanveteran'sbattlewithPTSDstillhauntsthoseheloved
By Tristan Ahtone for Al Jazeera America
Photos by Nicole Tung for Al Jazeera America
Produced by Joanna S. Kao
Edited by Vaughn Wallace, Katherine Lanpher
Published on Sunday, July 6, 2014
ROCK SPRINGS, N.M. — Her hair was still wet when she got to the hospital: dark brown locks that fell past the tips of her shoulder blades to the small of her back.
“I woke up at my normal time, 5:30, and I looked at my phone and I got this ugly feeling,” said LaTonya Johnson. “I thought I was dreaming.”
The text message on her phone read: I’m in the ICU. You’re probably sleeping, but I’m here.
Staff Sgt. Lonnie Al Watts was fighting a ventilator when she got to him. His heart rate was shooting up and down. He was hot, so she cleaned his face with a cool washcloth, and when the doctors told her he would need to be transferred to Albuquerque, she prepared to be there for him.
“I prayed with him, then I kissed his head,” said Johnson. “Rubbed his head again, and said, ‘I love you, be strong, I’ll be waiting for you in Albuquerque.’”
Watts never made it.
On Oct. 11, 2013, 37-year-old Watts was taken to the Gallup Indian Medical Center on the border of the Navajo Nation. He had blood clots in his lungs and pneumonia, and his heart — damaged by chronic and heavy alcohol use — was unable to provide oxygen to his body anymore.
Only a year before, Watts had been diagnosed with congestive heart failure. His doctor told him that if he didn’t stop drinking he would die, but he didn’t listen.
“Whatever happened in Afghanistan, it haunted him to drink,” said Johnson. “If this whole post-traumatic stress disorder [PTSD] wasn’t such a secret, I really feel like he would have got help, and the counseling probably would have helped him to quit.”
Approximately 10 percent of all Gulf War veterans suffer from PTSD. As many as two-thirds of veterans from Iraq and Afghanistan with PTSD may not be receiving treatment at all, and it’s estimated that up to 22 veterans commit suicide every day.
As soldiers return home — about 1.7 million over the past decade from the Middle East alone — their access to medical services depends largely on where they call home. For veterans in urban areas, health care centers are often only a few minutes away. In Indian Country, veterans can drive hours just to see a doctor, if they choose to do so.
Whether Watts would ever have sought medical help for his troubles will likely always be up for debate. However, it’s important to keep in mind that the Navajo Nation is about 27,000 square miles, and the closest VA medical centers that offer treatment for PTSD are in Albuquerque, New Mexico and Prescott, Arizona — both around two hours' drive from the reservation’s border.
Somewhere between mental health access and the perceived threat of stigma, many veterans do not get the help they need. That means that for families of returning combat veterans dealing with PTSD, there are two outcomes: surviving war and surviving the aftermath.
“I didn’t know what I was getting into,” said Johnson, who divorced Watts over his drinking but remained close with him until his death. “I didn’t know that he was going to suffer in silence.”
The two might be remarried now, Johnson said, if Watts had asked for help. If he had quit drinking. Instead, he refused to come home and compared his life with Johnson to a prison.
“I said, ‘What’s my prison?’” recalled Johnson.
“You’re going to make me stop drinking,” said Watts.
The sun was not yet up.
Ash covered the foot of the living room’s black wood-burning stove as it cracked and hissed at the cold morning air. Baby clothes dried on a chair by the stove's warm mouth — pink and pastel purple socks, blankets and onesies decorated with bears, cupcakes, polka dots and smiling butterflies.
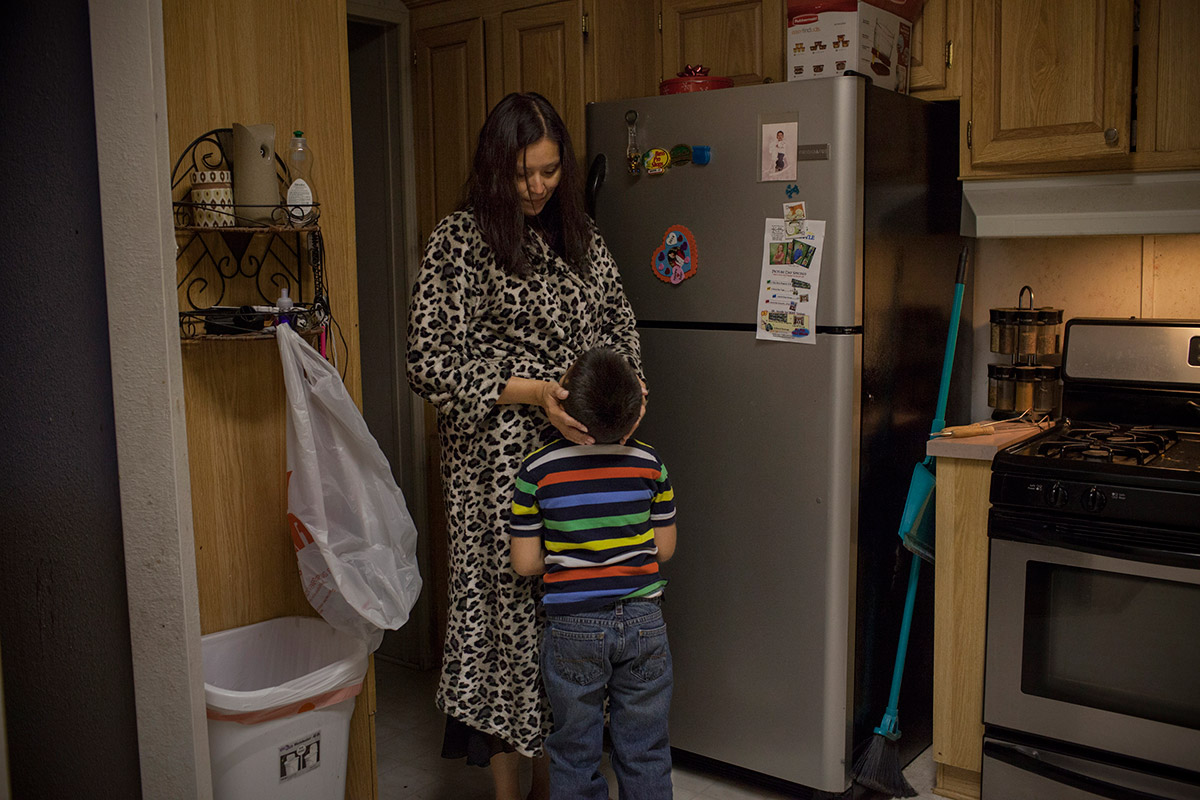
“You can’t stay home, you can’t,” said Johnson as she stood in the kitchen in her leopard-print bathrobe speaking to her 6-year-old son Landon. “I know you’re not sick.”
“My head hurts,” moaned Landon.
“Why do I feel like you’re not telling me the truth? What’s going on in school? What’s the matter?”
“Nothing,” said Landon, his denial punctuated with a sob.
By the end of the exchange, Landon knew he was going to school. He began to cry again.
“I think I need to really get on Landon’s bereavement counseling, because I notice he’s acting out more and more now,” Johnson said later. “Emotionally, I don’t think he can tell me how he feels.”
With only a few months passed since Watts’ death and funeral, adjustments had still not taken on any real form for any of the children: Jonathan and Jeremiah, from Johnson’s previous marriage; Ashley and Landon, born to Johnson and Watts.
Ashley, age 8, regularly saw her father in her dreams and occasionally traveled to Phoenix with him as she slumbered at night. Jonathan, the oldest at 19, was scheduled to leave for the Marine Corps in March, but changed his mind to stay at home and help his mother raise the newest addition to the family, 2-month-old Paisley, as well as his 14-year-old brother Jeremiah.
About a year earlier, when Watts was still alive, Johnson was diagnosed with cervical cancer. She went into a tailspin and began disappearing and drinking.
“I didn’t want reality and was escaping,” she said. “When I came to, I said, ‘Whoa, how did that happen?’”
When she came to, she also discovered she was pregnant with Paisley by another man. She called Watts — her ex-husband but still her closest confidante — to figure out what to do.
“He said, ‘You know we’re pro-life,’” said Johnson.
Watts accompanied her to every medical appointment she had for the pregnancy, but died before the baby was born. Six weeks after Watts’ death, Jeremiah and Jonathan’s biological father also died. After 19 years, Jonathan had finally become close with his birth father, and Johnson said he took it hard.
“They found his body south of Gallup,” she said. “Exposure from drinking.”
Jeremiah, on the other hand, was raised by Watts.
“He learned everything from him, he’s just a little him outside with tools and fishing and cooking,” said Johnson. “At the funeral for his own dad he said, ‘I don’t know him, I never knew him.’”
“We know that in the military as a whole, amongst veterans, those who live in rural areas definitely have worse access to care,” said Dr. Craig Bryan, a clinical psychologist and executive director of the National Center for Veterans Studies at the University of Utah. “It actually seems to be compounded among native groups that live on reservations, where it's even more rural than what we might typically think of as rural.”
Native Americans tend to have the highest rates of substance abuse disorders and high rates of suicide, and are more likely to engage in non-suicidal self-injury.
On top of those facts add statistics on PTSD in returning combat vets, and ridiculously large distances some Native veterans need to travel for services, and alternative methods to numb pain like drug and alcohol abuse, self-harm or even suicide don’t actually seem like out-of-the-question options.
Then add one more issue to the mess: stigma.
“I think the reason why we’ve not been very successful at overcoming stigma in the military is because we have not really looked at it from the perspective of this is a part of who they are,” said Bryan. “We’ve trained them to be this way, and it’s very difficult for someone to just abandon something that they value.”
In high-stress combat situations, no matter what happens, soldiers need to be able to keep functioning in order to survive. What that often means is compartmentalizing feelings, staying strong and resilient, and ignoring internal problems in order to stay alive.
That means when vets start having problems, whether it’s PTSD, substance abuse or family problems, they’re much less likely to reach out for help because it violates a sense of identity.
“To add to that struggle, military families buy into the culture. If you have been a spouse of a service member, you have a suck-it-up mentality,” said Kim Ruocco with the Tragedy Assistance Program for Survivors (TAPS). “You don’t talk outside your home about the struggles that your loved one is having for fear that people will view them differently, that they won’t get promoted, that they’ll lose their jobs.”
Since 9/11, TAPS has seen a steady increase in individuals and families looking for help after losing a veteran to suicide. Approximately 4,000 survivors of military suicide are currently in the organization’s database, and according to Ruocco, those who actually take the step to seek treatment are often at rock bottom.
“Their wife may have left them, they may have lost their job, they may have had criminal issues or addiction issues that have built up, and then it’s a complex matter,” said Ruocco. “But because of the stigma, they wait till when things are falling apart and it’s the very last option to ask for help.”
As for deaths from overdose, TAPS says that’s harder to quantify. Anecdotally, the organization has been seeing an increase in deaths by poisoning or accidents that aren’t counted as suicides. However, no data exists to help measure the issue.
“When someone’s engaging in self-destructive behavior, it's almost always because they’re not mentally well,” said Jill Harkavy-Friedman of the American Foundation for Suicide Prevention. “When you talk about things like addiction, like alcohol or drugs, those are really disorders that can be treated.” Staff Sgt. Lonnie Al Watts was a career soldier. He joined the Army at 18, never leaving until his death. He served tours in both Iraq and Afghanistan. He was never diagnosed with PTSD. In fact, he refused to even entertain the notion of seeing a doctor despite the growing number of alarming behaviors that had surfaced since he returned from Afghanistan.
Watts’ primary reason for refusing treatment: He was still on active duty with the New Mexico National Guard 1116th Transportation Company, and he was worried a diagnosis would affect his ability to work in the future.
“We in leadership positions have been trying to alleviate the stigma out there that if you claim PTSD that it’s going to be held against you,” said Lt. Cmdr. Anthony Rivera, one of Watts’ superior officers. “Our primary concern is that if somebody is suffering from that diagnosis of PTSD, we want to get them well and healthy for themselves and their families.”
Rivera and Watts held a few conversations about being deployed during their time working together, but for the most part, Watts was quiet about his time in Afghanistan. And while on the job, he was responsible, friendly and generally well liked, never showing any signs of a struggle with PTSD or even alcohol.
“He helped counsel some people with alcohol addiction and things like that,” said Rivera. “He helped coach and mentor people to get over that.”
According to Johnson, Watts would often get lost in conversation and zone out. When asked what was the matter, his usual answer was “You’ll never understand.” One night Johnson woke up when he had a nightmare and tried to choke her. On the Fourth of July, the family lit fireworks and Watts hid in the bushes, while the kids laughed at him, thinking he was playing a game. He often disappeared to drink after Johnson banned him from doing it in the house — sometimes for hours, then days and, eventually, months, which finally pushed Johnson to file for divorce.
Meanwhile, at work, Watts was an irreplaceable team member.
“I would characterize Sergeant Watts as a true American soldier,” said Rivera. “He did everything that was asked of him, no matter what. He was always there to help out any way he could. I would have a whole company of Sergeant Watts if I could.”
Johnson placed a triangular flag box along with military medals and photos of Watts on her dining room table.
“He wasn’t like other Native men from here,” she said. “He wasn’t shy. He was outspoken. He was different to my boys’ dad — he was shy and didn’t talk very much. When I met [Watts] he was just out there.”
Without Watts, Johnson says she gets lonely. Every Easter the two put baskets together for the kids, as a couple. This year she walked the garish pastel Easter aisles of grocery stores alone.
Johnson works as the executive secretary at the McKinley County sheriff’s office in Gallup. On weekends when the kids are out of school and Johnson doesn’t have to work, she does her best to get everyone out of the house. To escape the memories still living there, she says.
“Keeping busy is helping me, so I’m thinking keeping these guys busy is helping them. I haven’t really reached out to the resources that are out there like bereavement counseling for them,” she said. “I know they can’t tell me how they feel because they’re just still too small. I just need to make time for it.”
Somewhere between death, cancer, children and her future, Johnson finds a way to keep going — surviving the aftermath of war, one day at a time.
“I really wish that he got more help,” she said. “I feel like he could still be here raising the kids with me.”
Editor's note: This story has been updated to clarify the parentage of the youngest child born to Johnson.